Appendicitis
________________________________________________________________________
KEY POINTS
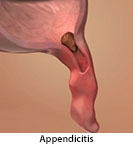
- Appendicitis is swelling and irritation of the appendix. The appendix is a small, finger-shaped pouch where the large and small intestines join.
- Appendicitis is usually treated with surgery to remove the appendix.
- Ask your provider how to take care of your child at home, what symptoms or problems you should watch for, and what to do if your child has them.
________________________________________________________________________
What is appendicitis?
Appendicitis is swelling and irritation of the appendix. The appendix is a small, finger-shaped pouch where the large and small intestines join. Healthcare providers are not sure what the appendix does, but when it is inflamed, it gets swollen and painful and can cause serious problems.
It is important to get treatment for appendicitis before the appendix ruptures. A rupture is a break or tear in the appendix. If an infected appendix breaks open, it can cause a life-threatening infection of the belly.
Because of the risk of rupture, appendicitis is considered an emergency.
What is the cause?
In most cases, appendicitis is caused by a blockage of the opening of the appendix by a piece of bowel movement. Sometimes it is caused by infection in the digestive tract.
What are the symptoms?
The symptoms can differ from child to child. They may include:
- Pain, usually starting near the bellybutton, then moving to the right lower side of the belly. The pain usually gets worse quickly and increases when your child moves or takes deep breaths.
- Loss of appetite
- Nausea and vomiting
- Constipation or diarrhea
- Trouble passing gas
- Fever, usually not very high
- Swollen, tight, or hard belly
Children under 10 are less likely to have the usual symptoms of appendicitis. Because of this, they may not get treatment right away, which makes it more likely that the appendix will rupture. Appendicitis is most common between the ages of 10 and 30. If you think your child may have appendicitis and is about to see his healthcare provider, do not let him eat or drink anything before he is examined.
How is it diagnosed?
Your healthcare provider will ask about your child's symptoms and medical history and examine your child. Your child may have the following tests:
- Blood tests
- Urine tests
- An ultrasound, which uses sound waves to show pictures of the belly
- MRI, which uses a strong magnetic field and radio waves to show detailed pictures of the belly
- CT scan, which uses X-rays and a computer to show detailed pictures of the belly
- Exploratory laparotomy: A surgeon will make small cuts in the belly with anesthesia to see if the appendix looks inflamed and should be removed. This is done sometimes after other tests do not give definite results for what is causing the symptoms.
If the diagnosis is not clear, your child may be watched closely in the emergency room or hospital for 12 to 24 hours to see if surgery is needed.
If your child’s provider does not keep your child in the hospital and sends your child home without surgery, your provider will tell you what symptoms or problems you should watch for and what to do if your child has them. Your provider will probably ask you to:
- Not give your child any pain medicine stronger than acetaminophen. Strong (narcotic) pain medicine could make it hard for you to know if your child’s pain gets better or worse.
- Not give your child any enemas or laxatives. These medicines increase the risk that the appendix will rupture if it is inflamed.
- Not give your child any antibiotics.
- Take and write down your child’s temperature every 2 to 4 hours.
- Contact your provider if any of your child’s symptoms get worse over the next few hours.
How is it treated?
Appendicitis is usually treated with surgery to remove the appendix. It is important to have surgery quickly before the appendix ruptures. People can live a normal life without an appendix.
Your child will be given general anesthesia to keep from feeling pain during the procedure. General anesthesia relaxes your child’s muscles and puts your child into a deep sleep.
Your child may have either one cut in the lower right area of the belly or 1 to 3 small cuts if your child’s healthcare provider uses a laparoscope, which is a lighted tube with a camera. If your child’s appendix is removed before it ruptures, your child will usually feel much better in a couple of days.
If the appendix has ruptured, infection can spread through your child’s belly, which is dangerous. Your healthcare provider may put a drainage tube in your child’s belly to help the infection drain. Your child will stay in the hospital after surgery to receive IV antibiotics and may need more than 1 surgery.
Treatment without surgery includes taking antibiotics to treat the infection. This treatment may be used if your child is not well enough for surgery or surgery is not available. Without treatment, appendicitis can be fatal. Close follow-up is important to make sure the infection is getting better and to decide if or when surgery is needed.
How can I take care of my child?
Follow the full course of treatment prescribed by your child’s healthcare provider. If an antibiotic has been prescribed, make sure that your child takes all of it according to instructions.
Ask your child’s provider:
- How and when you will get your child’s test results
- How long it will take your child to recover
- If there activities your child should avoid and when your child can return to normal activities
- How to take care of your child at home
- What symptoms or problems you should watch for and what to do if your child has them
Make sure you know when your child should come back for a checkup. Keep all appointments for provider visits or tests.
Last modified: 2017-11-08
Last reviewed: 2016-11-30