Skin Infection: Erysipelas and Cellulitis
________________________________________________________________________
KEY POINTS
- Erysipelas is an infection of the upper layers of skin. Cellulitis is an infection of the skin and the tissue under it. Both are caused by bacteria and need to be treated right away.
- The infection is treated with an antibiotic. If your child has an infection with a collection of pus, your child’s healthcare provider may drain the infection.
- Make sure that your child takes his or her antibiotic medicine for as long as your child’s healthcare provider prescribes, even if your child feels better.
________________________________________________________________________
What are erysipelas and cellulitis?
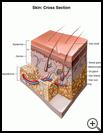
Erysipelas is an infection of the upper layers of skin. Cellulitis is an infection of the skin and the tissue under it. Both are caused by bacteria.
Skin infections are serious and need to be treated right away. Without treatment, the infection can damage skin tissues and spread quickly to other parts of your body. A skin infection that is not treated right away may lead to:
- Infection in your blood
- Tissue death (gangrene) and possible loss of a body part (amputation)
- Infection in your eyes, causing blindness
- Infection in your brain (meningitis)
- Death
What is the cause?
Many different types of bacteria can cause skin infections. The bacteria get into the body through a break in the skin.
Your child is more likely to get a skin infection if:
- Your child has a rash, cut, bite, sore, or IV drug injection site
- Your child has a medical condition such as diabetes, HIV/AIDS, or cancer that makes it hard for the body to fight infection
- Your child has an infection in the mouth, teeth, or sinuses
- Your child is obese
- Your child has swelling, especially in the legs, that lasts for many days
- Your child has had radiation treatment that left your child with a skin wound
- Your child has lymphedema, which can happen when the lymph system is blocked and cannot drain fluid from the tissues. This may be caused by:
- Infection
- Radiation
- Injury
- Cancer
- Prior surgery to remove cancer and nearby lymph nodes
- Problems with the lymph system that your child was born with
What are the symptoms?
Symptoms may include:
- Redness, swelling, and skin that feels hot to the touch
- Extreme tenderness or pain
- Swollen and tender lumps (lymph nodes) in the neck, armpits, or groin
- Red streaks that spread away from the wound or sore
- Fever and chills
- Fluid-filled sores
- Fast heart beat
How is it diagnosed?
Your healthcare provider will ask about your child’s symptoms and medical history and examine your child. Tests may include:
- Blood tests
- X-rays if there is a concern about a bone infection
- Ultrasound, which uses sound waves to show pictures of the tissue if there is a concern about a blood clot
- CT scan, which uses X-rays and a computer to show detailed pictures of the tissue if there is a concern about a sinus infection or brain infection
- MRI, which uses a strong magnetic field and radio waves to show detailed pictures of the tissue if there is a concern about a sinus infection or brain infection
- A culture, which is a swab of infected tissue or fluid that is sent to the lab and tested
How is it treated?
The infection is treated with antibiotic medicine taken by mouth. Your child’s provider may follow-up with you 2 or 3 days after the first visit to make sure the medicine is working. If the infection does not get better, or if the infection is serious, your child may need to stay in the hospital to receive antibiotic medicine through an IV.
If your child has an infection with a collection of pus, your child’s healthcare provider may drain the infection.
How can I take care of myself?
- Make sure that your child takes his or her medicine for as long as your child’s healthcare provider prescribes, even if your child feels better. If your child stops taking the medicine too soon, it may not kill all of the bacteria and your child may get sick again.
- Ask your child’s healthcare provider how to take care of the infected area. For example, your provider may recommend:
- Keeping the infected area up on pillows (above the level of the heart) when your child sits or lies down to decrease swelling and pain
- Putting a warm, moist towel on the reddened area
- Give your child pain medicine as directed by your provider.
- Give your child nonprescription pain medicine, such as acetaminophen, ibuprofen, or naproxen to treat pain or fever. Read the label carefully and give your child the correct dose as directed.
- Nonsteroidal anti-inflammatory medicines (NSAIDs), such as ibuprofen, naproxen, and aspirin, may cause stomach bleeding and other problems.
- Check with your healthcare provider before you give any medicine that contains aspirin or salicylates to a child or teen. This includes medicines like baby aspirin, some cold medicines, and Pepto-Bismol. Children and teens who take aspirin are at risk for a serious illness called Reye’s syndrome.
- Acetaminophen may cause liver damage or other problems. Do not give more doses than directed. To make sure you don’t give your child too much, check other medicines your child takes to see if they also contain acetaminophen. Unless recommended by your healthcare provider, your child should not take this medicine for more than 5 days.
- Ask your healthcare provider:
- How and when you will get your child’s test results
- How long it will take to recover from this illness
- If there are activities your child should avoid and when your child can return to normal activities
- What symptoms or problems you should watch for and what to do if your child has them
- Make sure you know when your child should come back for a checkup. Keep all appointments for provider visits or tests.
How can I help prevent cellulitis?
- Have your child wear gloves and protective clothing when playing, gardening, or working outdoors.
- Clean cuts, scrapes, and other skin injuries well with soap and water as soon as possible.
- Keep wounds and sores clean and dry. You may need to cover some wounds with a bandage to keep them clean and dry. Change bandages every day. Change them more often if they get dirty or wet.
- See your child’s healthcare provider for treatment as soon as possible if:
- Your child has a deep wound.
- Your child has a puncture wound or animal bite especially on the face, hand, or foot, or into a joint.
- Your child’s wound or sore shows signs of infection. Signs of infection include new or worse redness, swelling, pain, warmth, or drainage from the wound. Your child may have fever, chills, or a headache if an infection is getting worse.
- Your child may have a sinus or dental infection. Signs of an infection may include fullness, pressure, or pain in your face or head, toothache, headache, cough, sore throat, or fever.
- If your child has diabetes, follow your provider’s instructions for good skin care and keep your child’s blood glucose under good control.
Last modified: 2018-01-29
Last reviewed: 2018-01-25